eye floaters laser treatment
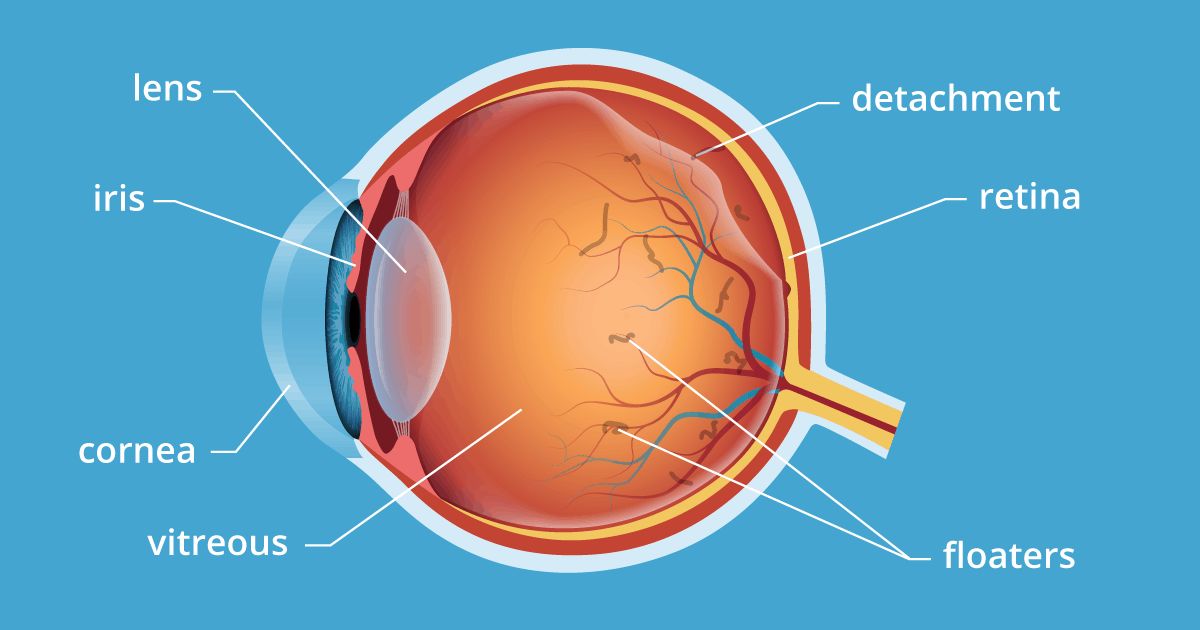
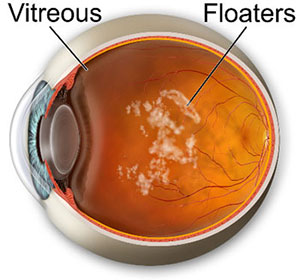
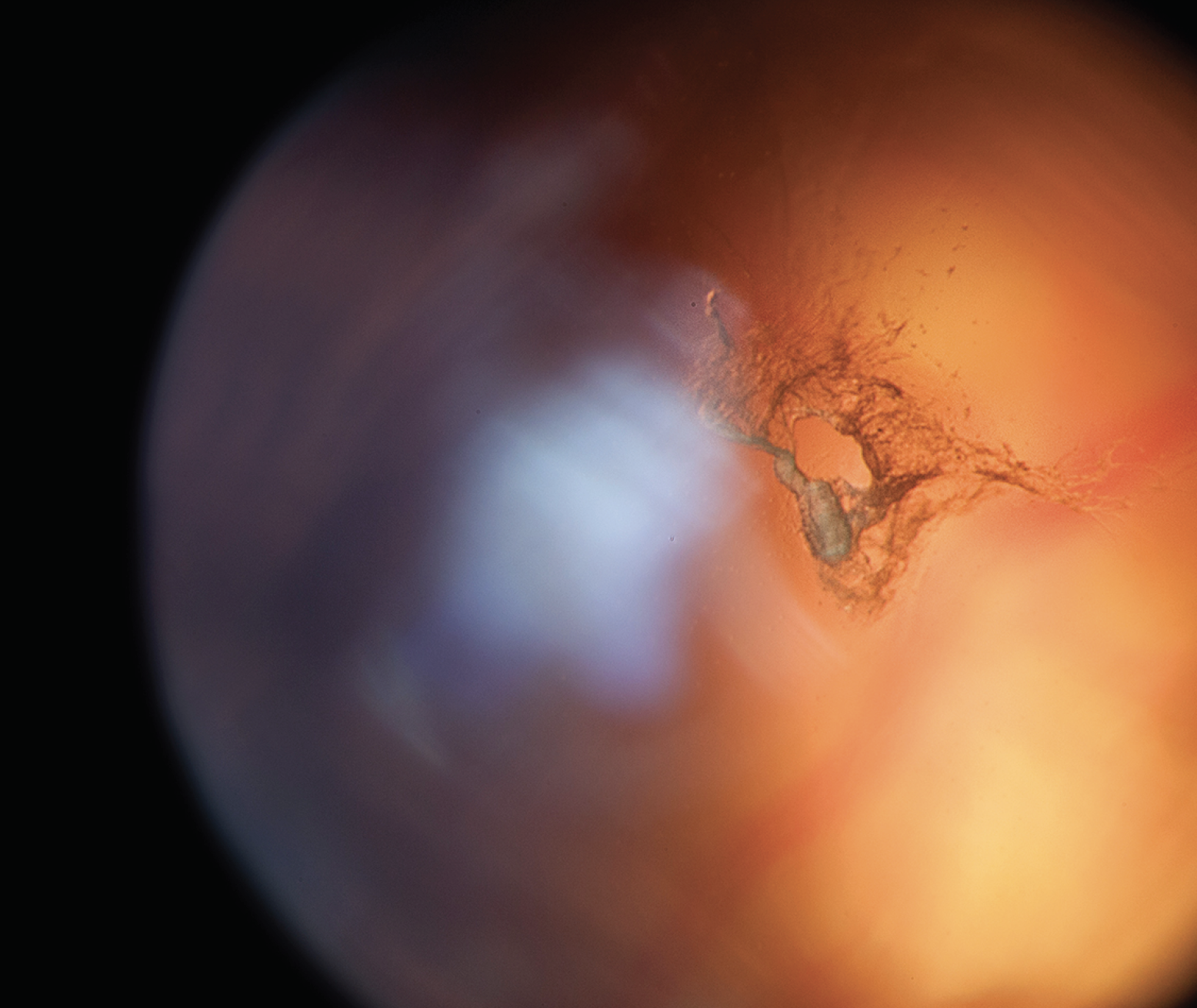
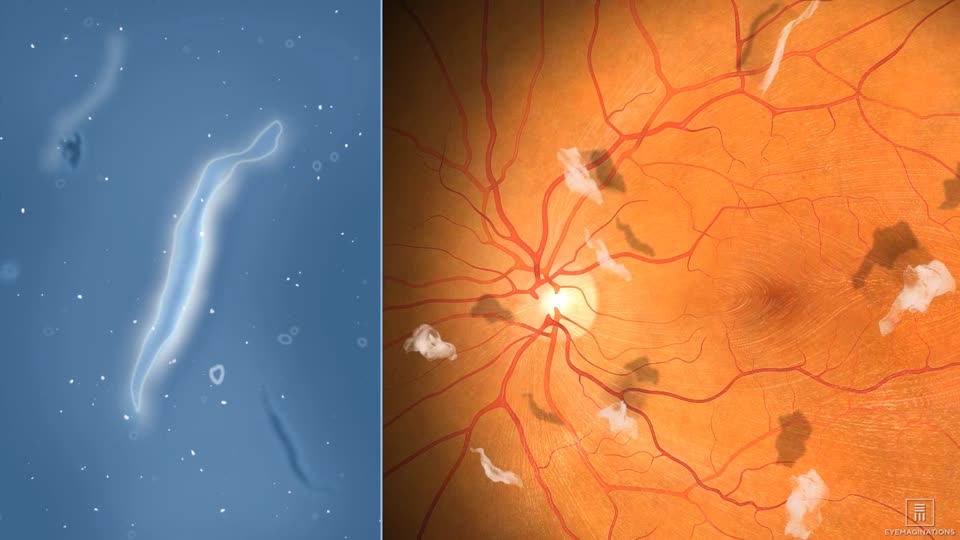
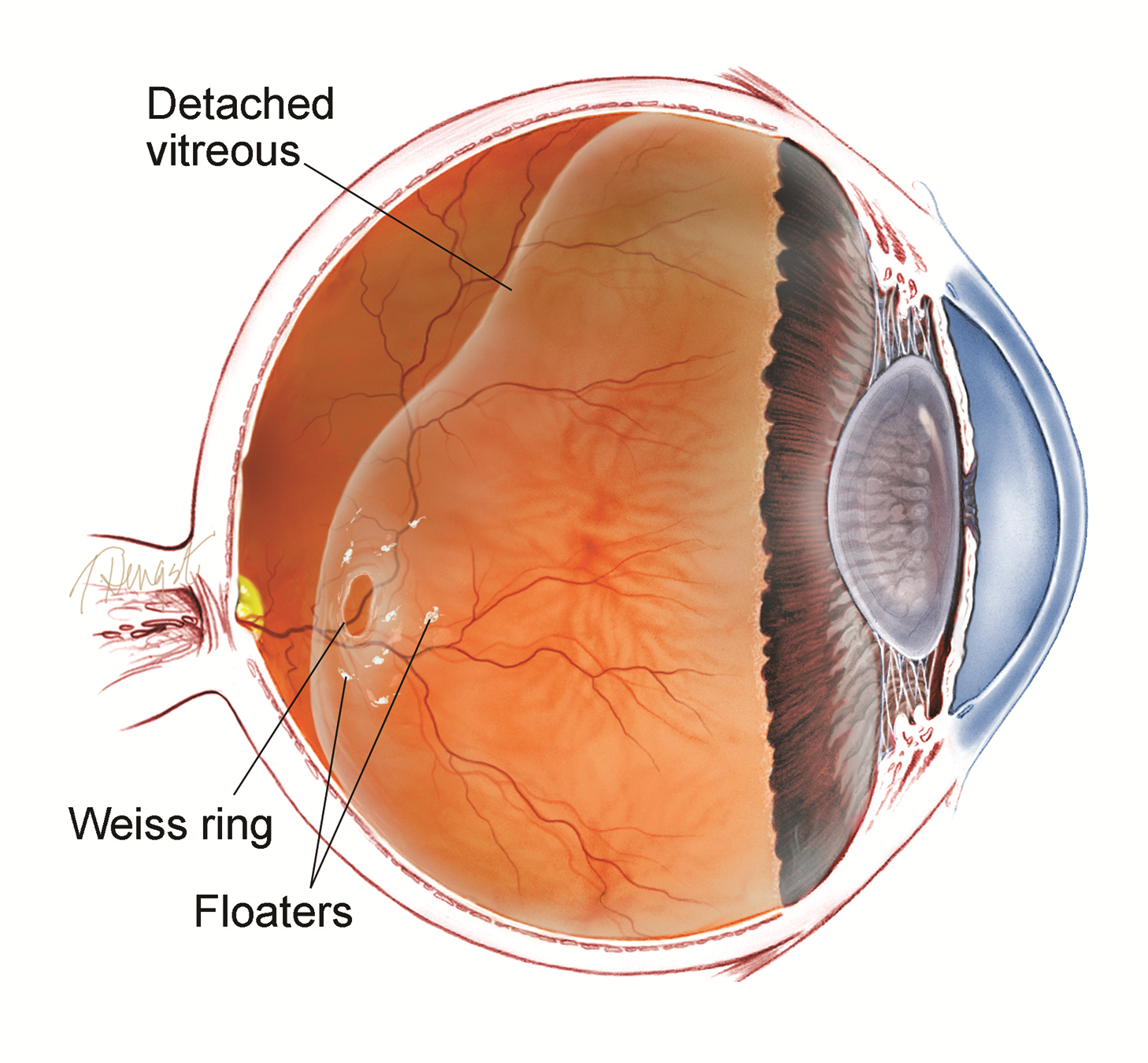
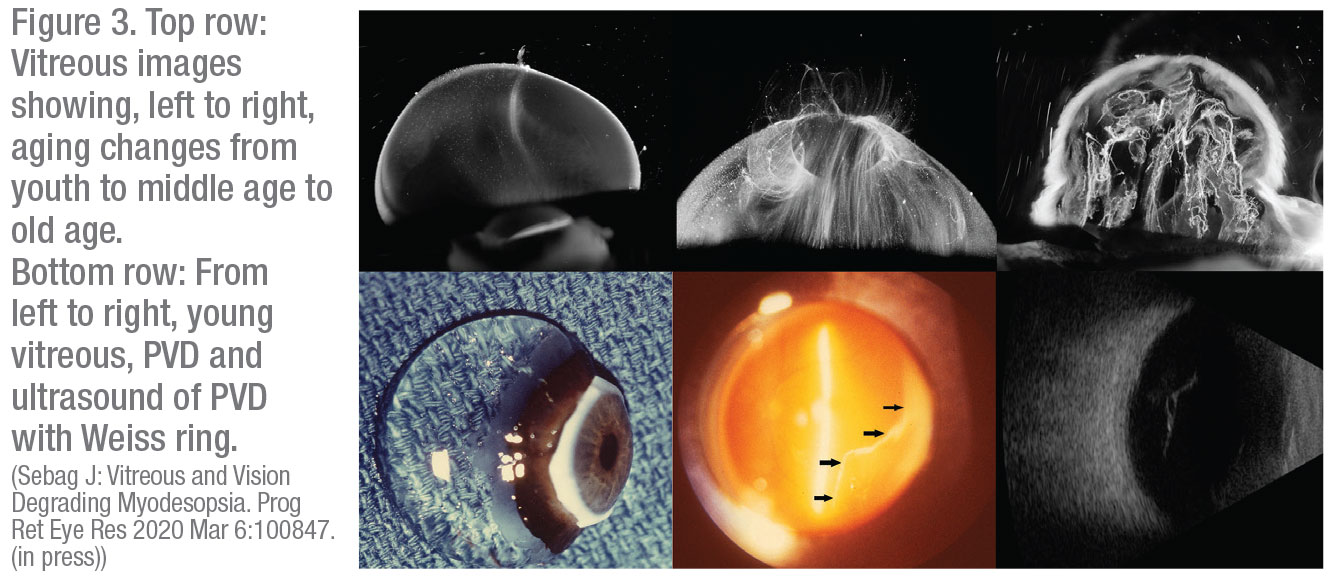
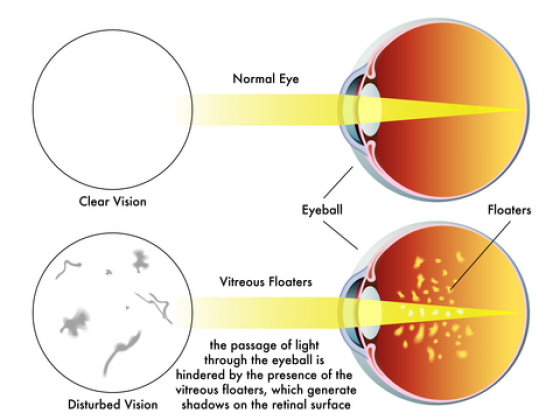
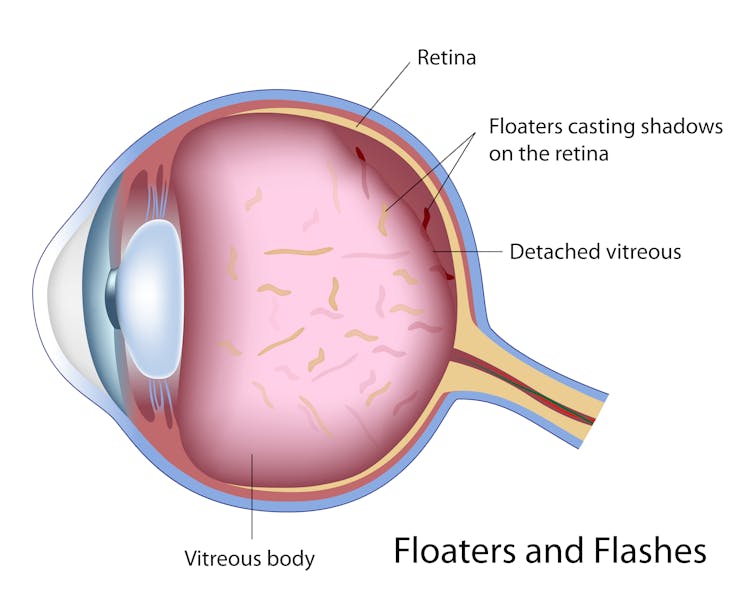
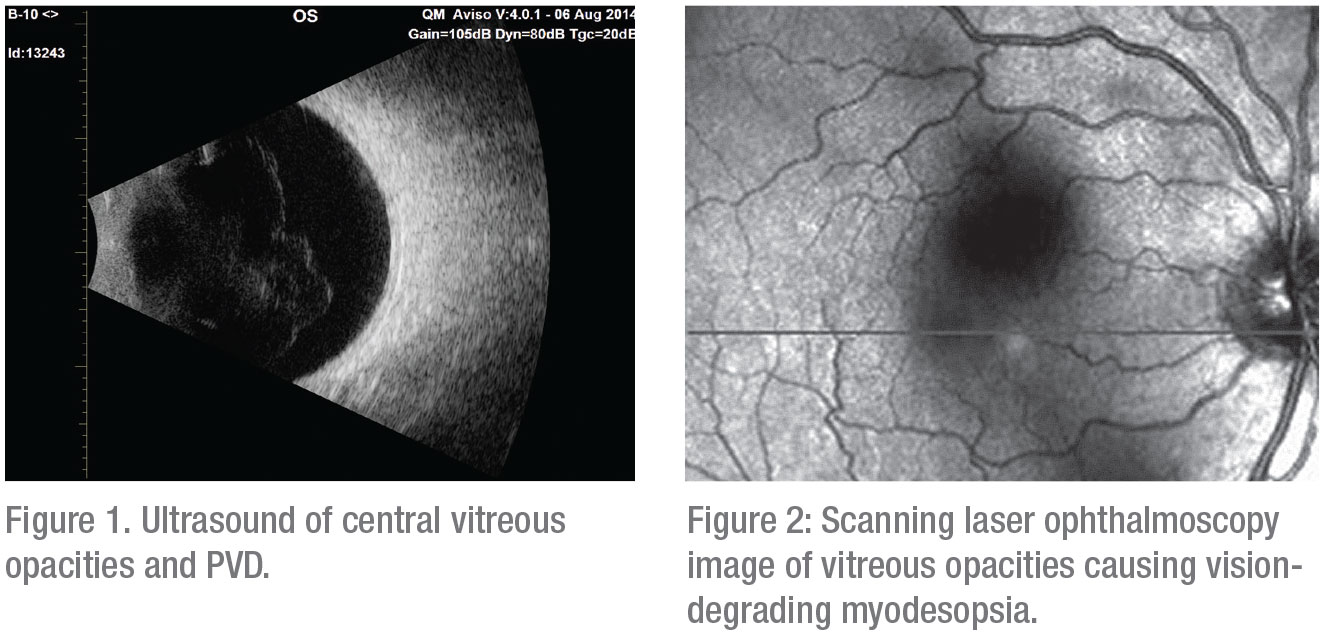
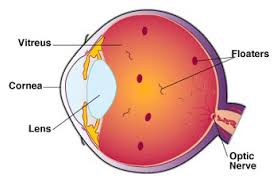
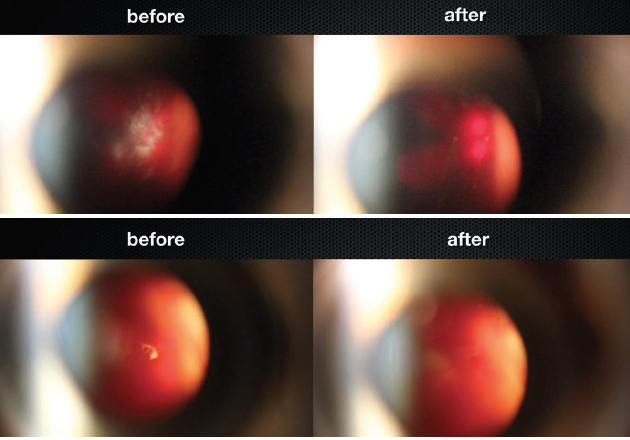
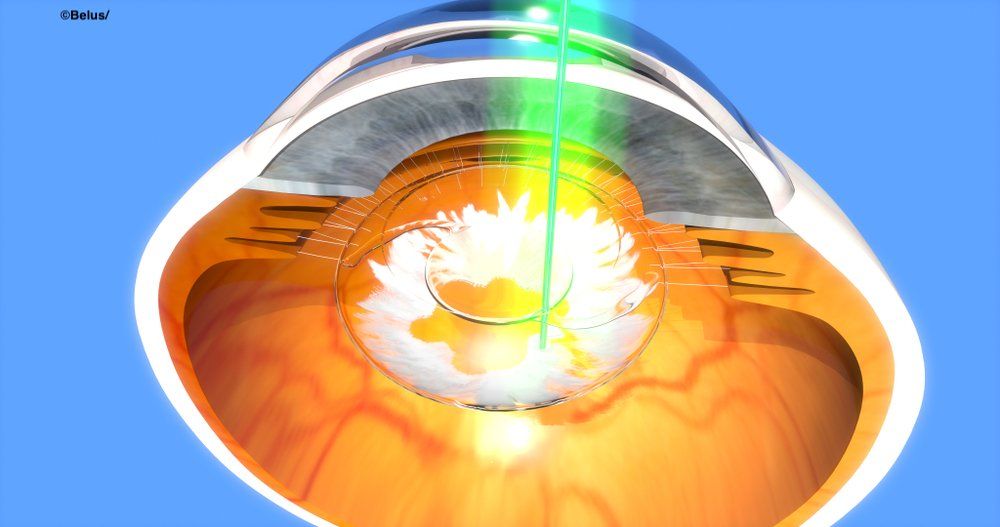
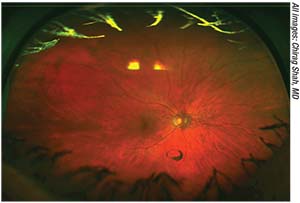
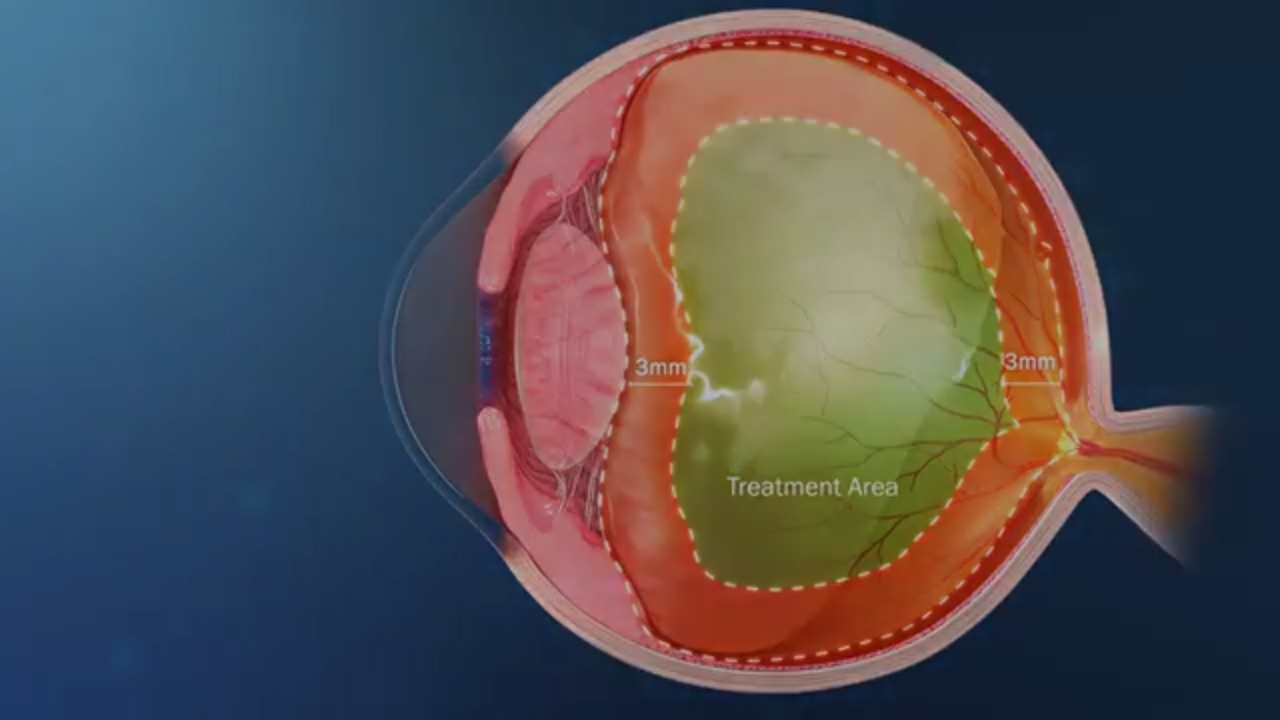
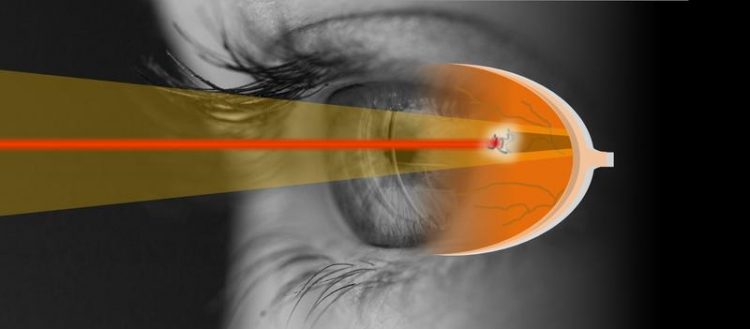
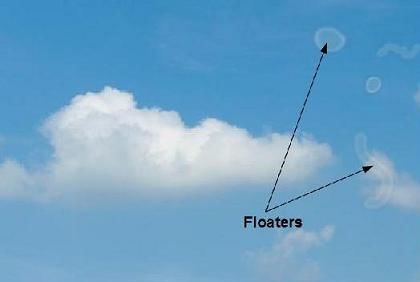
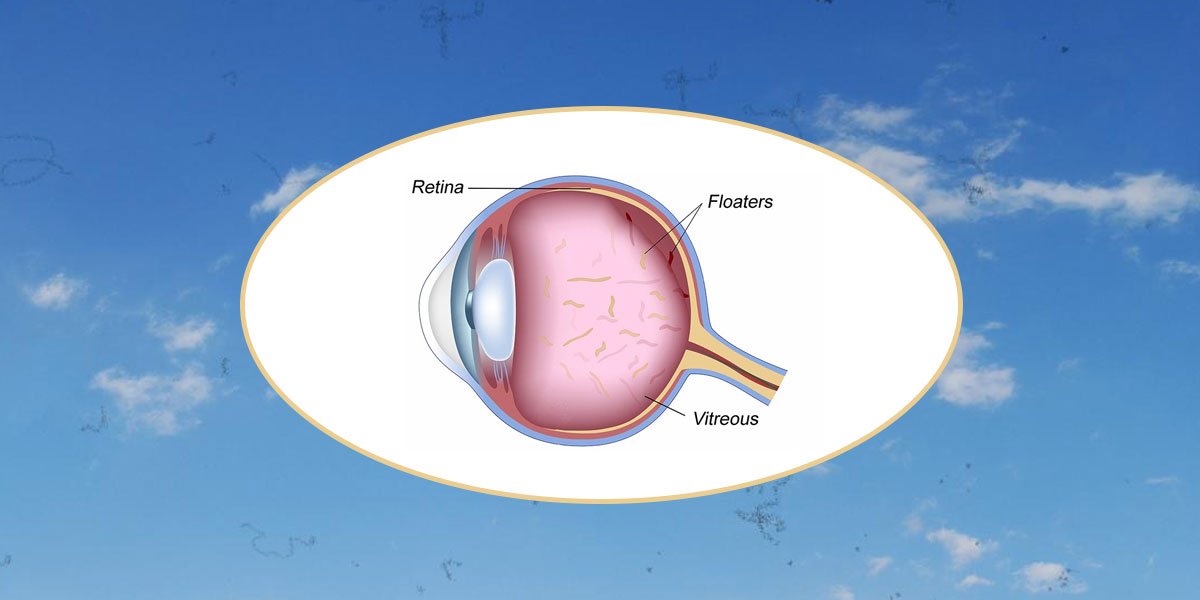
Treating – or not treating – Vitrious fleets Choose practically the practice of any ophthalmophyccultist and you will find patients complaining of vitreous flying. When, if ever, should these patients be treated? Like most of his colleagues, Chirag P. Shah, MD, MPH, with Boston Ophthalmological Consultants, prefers observation in 99.9% of these cases. "However," he said, "I think the paradigm is changing slowly. " A combination of a selection of more sophisticated patients and improved technology and techniques may be decreasing some concerns about the risks of surgery for vitreous floaters. And although a recent study1 by Dr. Shah also suggested that the YAG vitrosis can offer benefits to problem floaters, also raises questions about their effectiveness and safety, as well as the need for multiple costly sessions. Three vitreousal surgeons offer their perspectives on whether, and how, to treat vitreous floaters. Troublesome Vitreous Floaters Violent floaters can occur after a retinal, retinopexy, spinal or vitreous hemorrhage associated with a tear, said Gaurav K. Shah, MD, with the Retina Institute in St. Louis, Mis-souri. But most of the patients who experience vitreous floats fall into 2 groups: those who have a subsequent vitreous detachment (PVD) or myopic vitreopathy. PVD and myopic vitreopathy. People aged 50, 60 or 70 can develop a PVD and have more significant floats, said Dr. Chirag Shah. "Most of the time, patients can face them because brain neuroadapts. But a certain percentage of patients are still bothered by floaters." People aged 20 and 30 can also develop opacities in their vitreous as a result of myopia, said Jerry Sebag, MD, at the VMR Institute for Macula Retina Vitreous in Huntington Beach, California. Impact of light. "Because the impact is greater in bright light, individuals with floaters — often young people — are theoretically complaining about the inability to work long hours on computers," said Dr. Sebag. In addition, the reflections of snow, the bright skies, and looking at the ocean can be annoying. "I have had patients who tell me they have stopped camping, fishing or skiing because they no longer find these pleasant activities. Some even tell me they can't wait to sleep at night." Why worse for some? Why some people are more distressed than others are not fully understood, Dr. Sebag. It may be connected to more than 1 factor, he said, like biochemistry and the effects of aging, genetics, hormones and neuroadapt capacity. "For example, some have a dense subsequent vitreous cortex, and these people cannot adapt well to their floats." What is clear, he said, is that many of these patients feel ignored by the medical profession. "What you're explaining may not fit perfectly into our diagnostic boxes, but that doesn't mean you don't have a problem." Evaluating the vitreous floats Less than 5% of the patients of Dr. Chirag Shah complains about floaters. Since not all floaters are created equally, he said, it is important to demonstrate a correlation between what the patient is experiencing and what the doctor is seeing. "Deciding who to treat ends up being the key to success." Why do doctors underestimate the severe symptoms of vitreous floaters? "One reason is that we usually check the visual acuity and the visual fields of patients," said Dr. Chirag Shah, "but we do not check the contrast sensitivity, which can be degraded by significant floats." In addition, floaters can enter the central vision of the patient, affecting their ability to read or drive, but actors rarely check the reading speed. Dr. Sebag was the first to discover that patients with significant vitreous floats are bothered with a decrease in the function of contrast sensitivity. 2-4 Accused the term "degradant vision disease" to help distinguishing debilitating floaters from those who are relatively benign. "The creation of specific questionnaires for vistress, structural evaluations with ultrasound and functional evaluations of contrast sensitivity (CSF) give me the ability to diagnose degrading vision vitreopathy and make me more comfortable in offering treatment," he said. Questionnaire of floaters. Dr. Sebag and his colleagues designed a detection tool called the Vitreous Floas Functional Questionnaire (VFFQ) to help assess the impact of the floaters on the quality of life of patients. "We have shown a statistically significant correlation between the VFFQ and the National Institute of Eyes (NEI) A question of visual function, a gold standard to evaluate vision in more general terms," he said. In addition, there is a high correlation between the results of VFFQ and CSF and the density of the vitreous body as assessed by ultrasound. Contrast sensitivity function. A CSF evaluation provides a functional evaluation of the impact of vitreous opacification (as well as the cornea or lens) on the vision, measuring the ability to distinguish the shades of grey, Dr. Sebag said. One of his studies found that patients with annoying floats had a 67% reduction in the CSF compared to adjusted age controls. 2 "These days, I never operated on someone with normal CSF," Dr. Sebag said. More than 140 patients with abnormal CSF who have performed the vitretomy reached the normal CSF within a week of surgery. 2-4 Dr. Sebag has followed these patients for an average of almost 3 years; during this time, their CSF has remained normal. Quantitative ultrasound (QUS). Dr. Sebag also advocates the use of quantitative ultrasound, which gives an index of the structure of the vitreous body. "The quantitative ultrasound measures we do clearly show that the greater the density of the vitreous, the more patients are bothered by their floats," he said. He added that QUS is also a useful way to show patients what is going on within their eyes and to evaluate the effectiveness of vitrectomy. A wide-angle color photograph. In your clinical trial, Dr. Chirag Shah used wide-angle color photography to visualize floating. "Often, patients looked at their color photographs and said, 'That's the floater as a bug that keeps coming in and coming out of my vision'," he said. "If a patient had significant symptoms, but photography was crystalline except for a few normal vitreous wisps, that patient may not be easy to satisfy. "OCT. To evaluate the floaters, Dr. Gaurav Shah takes optical coherence tomograph (OCT) infrared video images. "This allows us to see what patients are seeing," he said. "If I do a video analysis and I don't see much, the patient's symptoms are not eye, and I won't treat them with vitectomy. If patients really have something, it is a very dramatic demonstration of their symptoms."Vitrectomy for Troublesome Floaters "Vitrectomy is valuable for some floating paths, but I tend to reserve it only for those with the most weakening floats due to the potential side effect profile," said Dr. Chirag Shah. Vitretomy is invasive, accepted Dr. Gaurav Shah. "But it has evolved and has been claimed for improvements in technology and technology. My patients have been ecstatic with the results, although it is first critical to determine that they are truly symptomatic and have been given the opportunity of neuroadapt or to allow the floats to resolve." Dr. Sebag uses the VFFQ, CSF and QUS to select the best candidates for vitretomy. "I don't take the surgery slightly," he said, explaining that he has performed only about 200 surgical floating cases in more than 8 years. "I rarely meet someone and say, 'Let's operate.' In fact, he said the average time was the first start of symptoms and surgery is more than 30 months. Dr. Gaurav Shah uses slightly different criteria to exclude patients. "Exhibited to patients who are factual, who have 360 degrees of zeal or many peripheral retina problems, or who have expectations that are far beyond what surgery can provide." To help assess expectations, ask your patients, "If you're driving on a road and the whole windshield is clear except for a small point, does that bother you?" If the answer is yes, it is more concerned about the ability to please the patient with surgery. Vitretomy risks. "With vitrectomy, you're creating 3 holes in your eye," said Dr. Chirag Shah, "which carries a small risk of infection." Vitretomy also accelerates the formation of cataracts, due to the increase in oxygen concentration in vitreous cavity after the elimination of the vitreous. "But for me, retinal detachment is the most worrying, with reports published as high as 10.9%," he said. Presenting findings of 151-eyed vitectomy at the annual meeting of the 2016 Academy, Dr. Sebag did not report cases of endophthalmitis or hypotony; 1 case each of glaucoma, cystoid macular edema, and retinal breakage; 2 cases of retinal detachment that were surgically corrected; and 6 cases of vitreous hemorrhage, all spontaneous. Risk reduction. Dr. Gaurav Shah has found that discernment in patient choice has led to fewer complications. Operating in 5 to 10 floating patients last year, he has not had patients experience retina tears or detachments. The key, he said, is the 27-caliber topic vitectomy, which minimizes complications with blocks and intraoperative problems. Dr. Sebag also credits the development of sutureless and small-calibre vitretomy to reduce risks, as well as a couple of other techniques. Reduce the risk of endofalitis. To this end, Dr. Sebag creates highly beveled incisions and uses non-huge probe for the extraction of cannula. Leave a little vitreous. "I have modified my approach by leaving a few millimeters of vitreus behind the lens. Antioxidants in the vitreous gel help to mitigate the formation of cataracts," Dr. Sebag said. He and his colleagues compared the incidence of cataract using this modified approach to a wide vitretomy, which is used in the University of Amsterdam. At 24 months, the incidence of cataract was 35 per cent with the modified approach and 87 per cent with the broad approach. The time until the formation of cataracts was also 5 more months with a limited vitectomy. 5 Two philosophies in surgical PVD. The younger patients have vivid floaters because collagen is connected in the vitreous body, not by PVD, Dr. Sebag said. To reduce the risk of tears in these patients, it recommends simply removing the central vitreus and not separating the posterior vitreus from the retina. On the contrary, Dr. Gaurav Shah said he always creates a complete PVD because he is concerned that the attraction of the residual cortical vitree can cause problems in the future. That has not been the case in Dr's experience. Sebag of 200 cases, where only 1% experienced retina detachment. YAG laser vitreolisis for troublesome Floaters Before performing the first randomized clinical trial of YAG vitreolisis for symptomatic Weiss ring floats, Dr. Chirag Shah wondered if lasers could provide a niche between performing the vitectomy and doing nothing. "I was very skeptical entering the study, and I'm not doing this procedure," he said, "but the study has shown me that vitreolisis YAG may have some value." In the trial, 54% of the laser group reported the improvement of the symptom after 1 treatment. In addition, no differences were identified in adverse events between laser groups and sham.1 "We need to conduct longer-term studies to determine the best candidates and the number of necessary treatments, as well as the real risks and benefits of the treaty," said Dr. Chirag Shah. Although more than half of the patients in the Dr. Chirag Shah reported a significant or complete solution of its vitreous floats, only about one third of the patients in a previous study of Delaney et al. similar results.6 "We use greater laser power in our study, which can explain the differences in the response," said Dr. Chirag Shah. "In a lower power, you are making more fractionation, but when you increase power, form plasma and you can see the tissue vaporize in gas bubbles." Dr. Sebag, however, contests this claim, saying that the YAG laser does not vaporize the tissue. "YAG lasers are photodisruptors," he said. "Take something big and break it into smaller pieces." Anomalous? In the Dr.'s essay. Chirag Shah, 8 patients auto-reported zero improvement of a 100 scale despite color photography showing significant or complete objective improvement. "Some patients recognized that the float had gone practically, but a small stain that was mobile, possibly more than before, bothered them in the same degree as their great floater," he said. Exclusion criteria. In the Dr.'s study. Chirag Shah, the following patients were excluded: those with better corrected visual acuity of Snellen worse than 20/50 in the un studied eye; history of retinal tear, retinal detachment, uveitis, diabetic retinopathy, macular edema, occlusion vein retina, or afakia in the study; and history of laser glaucomacular. "For my knowledge, only a handful of doctors are making YAG vitreolisis, and with variable results," said Dr. Chirag Shah. Without a dedicated insurance code, the procedure is done off the label, he said. In your study, Dr. Chirag Shah only did 1 treatment session because he could not treat patients with 2 shaving lasers without unmasking them. "In the real world, patients may require 2 or more laser sessions to vaporize most of their floats." With YAG vitreolysis, there is a risk of glaucoma, retinal tear, retinal detachment, cataract if you hit the lens, and retinal damage if you hit the retina, said Dr. Chirag Shah. To minimize the risks of lens or retina damage, it recommends ensuring a safe distance between the laser focal point and the retina and the crystalline lens. In the study, it required the Weiss ring float to be 5 mm after the posterior capsule of the crystalline lens and 3 mm previous of the retina, measured by ultrasonography B-scan. Dr. Gaurav Shah has not personally used the laser for the floaters, but is concerned that it may be a prolonged procedure, and he noted, "Even though the laser appeared fairly safe in this recent laser study, it may have potential inconveniences." He added, "It is important to remember that the vast majority of patients do not require intervention. However, there are those who are truly symptoms and may require a procedure, and, more importantly, [who can benefit from] a conversation that recognizes their pathology." ___________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________ JAMA Ophthalmol. 2017;135(9):918-923.2 Sebag J et al. Retina. 2014;34(6):1062-1068.3 García GA et al. I'm J Ophthalmol. 2016;172:7-12.4 Milston R et al. Surv Ophthalmol. 2016;61(2):211-227.5 Yee KMP et al. Ophthalmol Retina. 2017;1(2):154-157.6 Delaney YM et al. Ojo (London). 2002;16(1):21-26.______________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________ Sebag is a vitreo-retinal specialist at the VMRInstitute for Vitreous Macula Retina in Huntington Beach, Calif., and a professor of clinical ophthalmology at the Doheny Eye Institute in Los Angeles. Relevant financial information: Abbott Labs: C; Johnson & Johnson: C. Dr. Chirag Shah is a retina specialist at the Boston Ophthalmological Consultants; co-director of the combined Tufts New England Medical Center/Ophthalmic Consultants ofBoston vitreoretinal surgery Partnership; and assistant professor at Tufts University School of Medicine, all in Boston. Relevant financial information: Ellex: L.Dr. Gaurav Shah is a retina specialist and co-director of the retina scholarship at the Retina Institute in St. Louis, Mo. Relevant financial disclosures: None. For full disclosure and disclosure key, see below. Full financial disclosures Dr. Sebag Abbott Labs: C; Johnson & Johnson: C; Roche Pharmaceuticals: C. Dr. Chirag Shah Ellex: C; Genentech: S; Johnson & Johnson: S; National Eye Institute: S; Ophthalmic Consultants-Boston: E; Regeneron: S. Dr. Gaurav Shah Allergan: C,S; Bausch + Lomb: L; DORC: C; Regenerated: C,L; Spark: C. Outreach category Code Description Consultant/Advisor C Consultants fees, paid counselings or fees to attend a meeting. Employee E Employed by a commercial company. Table of speakers L Fees or fees, travel fees or refunds when speaking at the invitation of a business company. Equity owner O Possibility of ownership and stocks in public or private commercial enterprises, excluding mutual funds. Patents/Royalty P Patents and/or royalties for intellectual property. Grant support S Grant support or other financial support to the researcher from all sources, including research support from government agencies (e.g. NIH), foundations, device manufacturers and/or pharmaceutical companies. Full financial disclosures Dr. Sebag Abbott Labs: C; Johnson & Johnson: C; Roche Pharmaceuticals: C.Dr. Chirag Shah Ellex: C; Genentech: S; Johnson & Johnson: S; National Eye Institute: S; Ophthalmic Consultants-Boston: E; Regeneron: S. Dr. Gaurav Shah Allergan: C,S; Bausch + Lomb: L; DORC: C; Regenerated: C,L; Spark: C. Outreach category Code Description Consultant/Advisor C Consultants fees, paid counselings or fees to attend a meeting. Employee E Employed by a commercial company. Table of speakers L Fees or fees, travel fees or refunds when speaking at the invitation of a business company. Equity owner O Possibility of ownership and stocks in public or private commercial enterprises, excluding mutual funds. Patents/Royalty P Patents and/or royalties for intellectual property. Grant support S Grant support or other financial support to the researcher from all sources, including research support from government agencies (e.g. NIH), foundations, device manufacturers and/or pharmaceutical companies. Dissemination CategoryCodeDescription SITESFOLLOW THE ACADEMY Public Professional Doctors " Patients Museo del Ojo
Eye floaters: Laser treatment, symptoms, causes
Not Sure if You Have Floaters & Flashes: Get Checked in Neenah WI - OptiVision Eye Care
YAG Laser Vitreolysis for eye floaters | Assil Eye

Laser Surgery for Eye Floaters Treatment (Laser Vitreolysis) - YouTube

Floaters | LESH

YAG Laser Treatment of a Dense Vitreous Eye Floater. The Floater Doctor - YouTube
Laser Floater Removal | Boston Eye Group
Laser Floater Removal | Zion Eye Institute
Our Book - Laser Treatment of Eye Floaters - Laser Treatment of Eye Floaters
Vitrectomy for Floaters - The American Society of Retina Specialists
Daring to Treat Floaters

EYE FLOATERS: Causes, symptoms and treatment / COC
Eye Doctor in Chapel Hill | Eye Disease Treatment | Floaters

Eye floaters treatment - does it exist? - Dr Claudine Pang
Eye Floaters (Flecks & Spots in the Eye)

Vitrectomy for Floaters - La Jolla, CA Eye Care Vision Correction

Yag Laser Vitreolysis for Vitreous Floaters - Tanner Eyes
The laser beam that can get rid of those pesky eye floaters
Daring to Treat Floaters
FLOATERS and TREATMENT | Premium Vision Surgical Centres
What are Eye Floaters? - Laser Treatment of Eye Floaters

Using laser treatment to target eye floaters

YAG laser offers safe option for floaters

Videz žoga Lažne floaters after laser eye surgery - body-n-coach.com
CRSToday | The Evolving View of Laser Vitreolysis
Laser-heated nanoparticles bust eye "floaters"
Laser Floater Treatment (Laser Vitreolysis) - Specialist Eye Surgeons SA

large white floater in cat eye - natural things to help eye floaters.eye surgery to remove floater… | What causes eye floaters, Floaters eye, Eye floaters treatment
FLOATERS and TREATMENT | Premium Vision Surgical Centres
Advances in floater treatment

What Causes Eye Floaters? - Signs, Symptoms, Treatments | Health.com

Eye Floaters Laser Treatment Cost In India | Eye floaters cure, Eye floaters treatment, Eye floaters causes

What are Eye Floaters? Symptoms, causes and treatments
Vitreous Floaters: What Can Be Done?
Eye Floaters Treatment | Vitreolysis | CFS
Yag Laser Vitreolysis for Vitreous Floaters - Tanner Eyes

The laser beam that can get rid of those pesky eye floaters
Clear vision – project for safer laser treatment of floaters started - Innovations Report
Treatment of Eye Floaters! - By Dr. Radhika A (Md) | Lybrate
Are Eye Floaters Normal? Here's What You Need to Know | Island Retina
Posting Komentar untuk "eye floaters laser treatment"